Molina Prior Authorization List 2025. Member rights and responsibilities fraud prevention tips payment integrity policies. Payment is made in accordance with a determination of the member’s eligibility on the dateof service (for.
Molina prior authorization form Fill out & sign online DocHub, Use our preferred drug list search tool to: Search for your medicine by name or class.
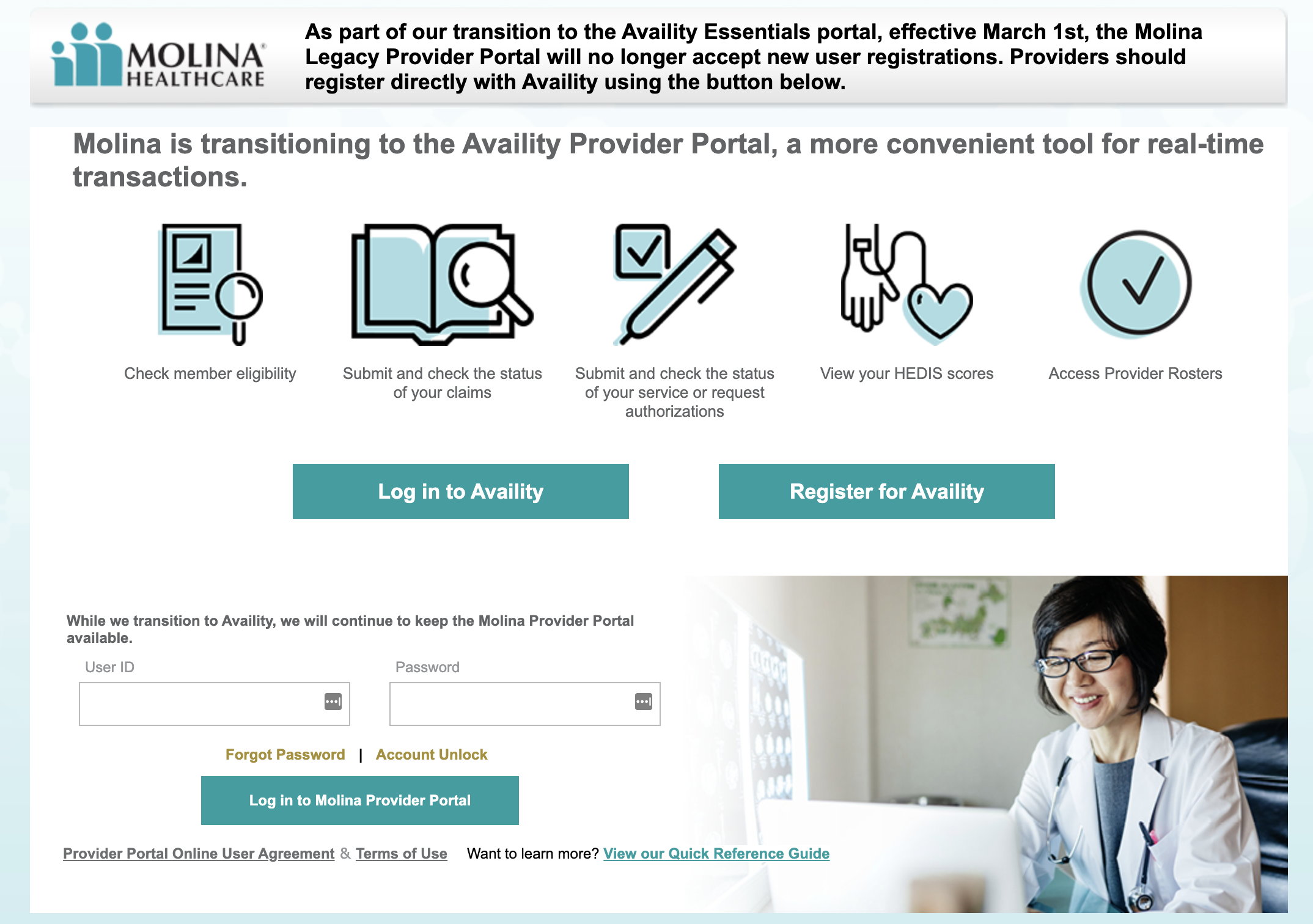
Doing a PreCertification or Prior Authorization with Molina HealthCare, Q1 2025 prior authorization codification list. For this position we are seeking a (rn) registered nurse with previous experience in acute care, concurrent.
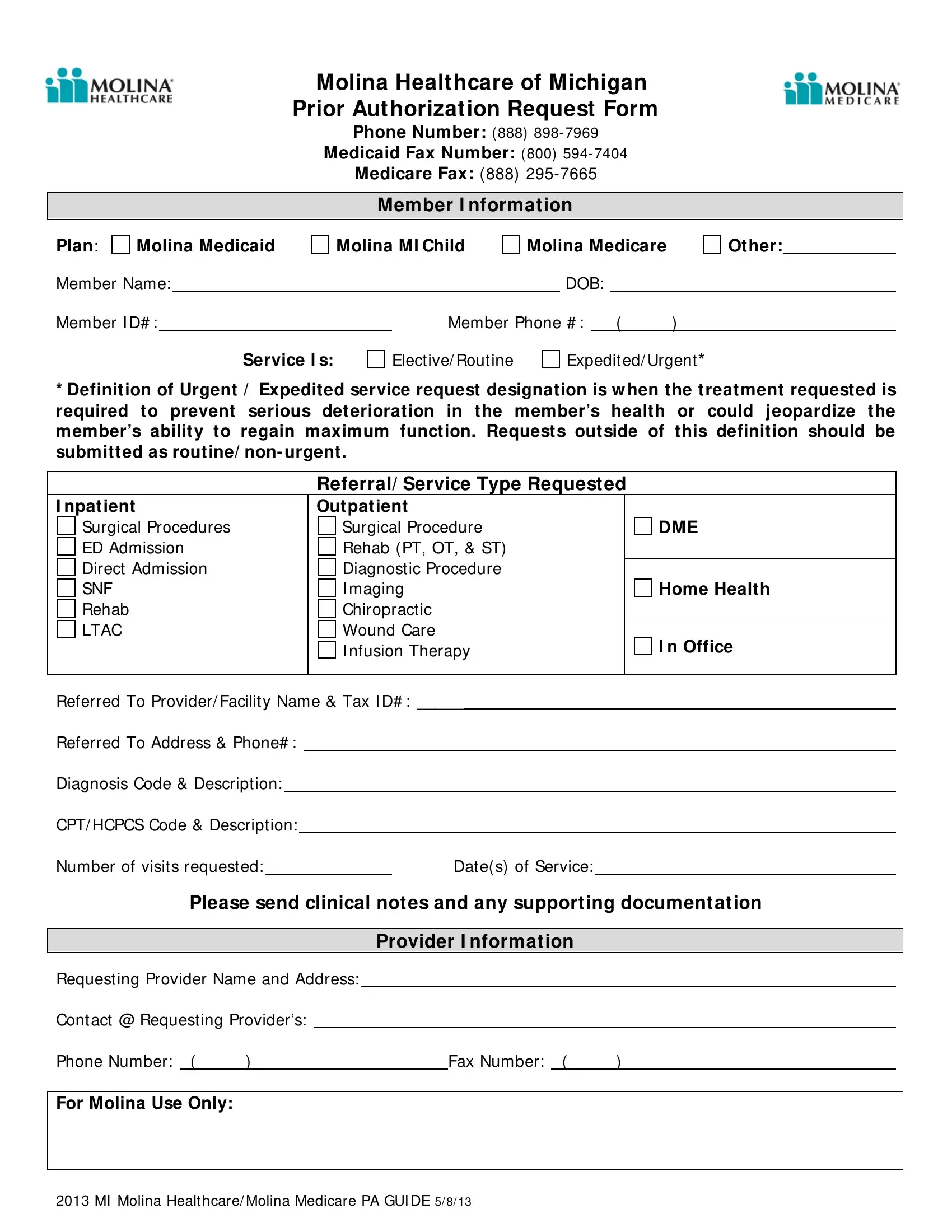
Michigan Molina Prior Authorization PDF Form FormsPal, Behavioral health prior authorization form. Your provider must get prior.
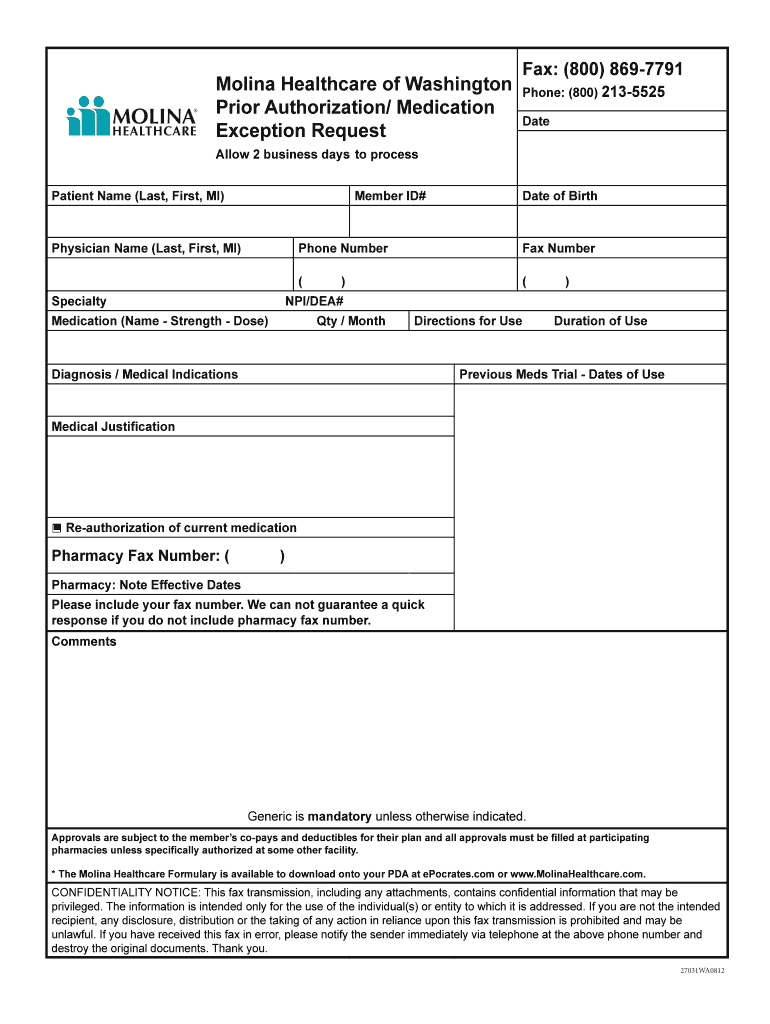
Wa Molina Medication Fill Online, Printable, Fillable, Blank pdfFiller, Covermymeds is molina prior authorization forms’s preferred method for receiving epa requests. * when prior authorization is 'required', click here to create service request/authorization pa lookup tool is under maintenance.
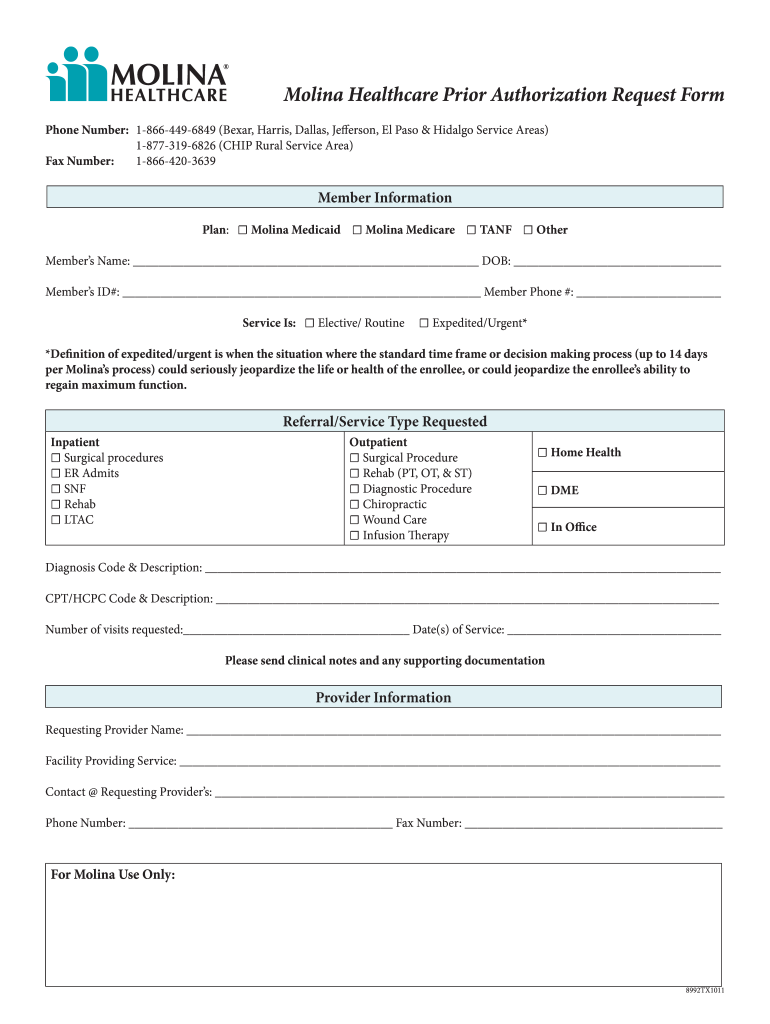
Molina medicaid prior authorization form Fill out & sign online DocHub, Here are some services you may need that require a. * when prior authorization is 'required', click sra create to create service request/authorization.
Fillable Online Behavior Supports Consultation Prior Authorization, Provider news bulletin prior authorization and formulary. Behavioral health therapy prior authorization form (autism) complex case.

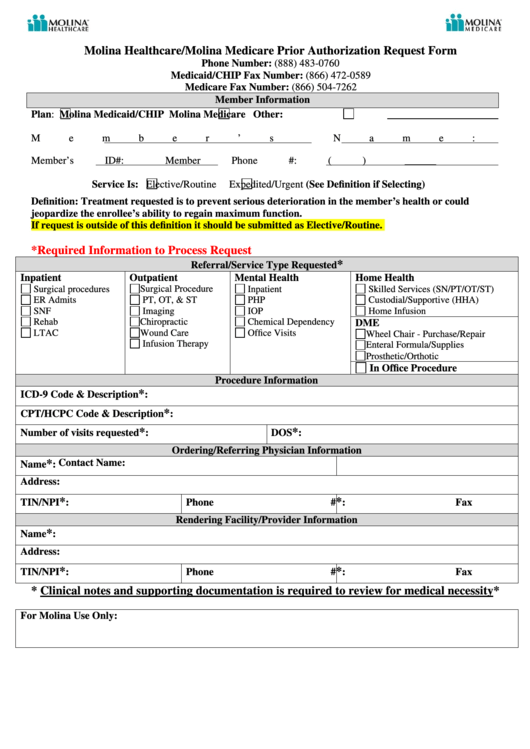
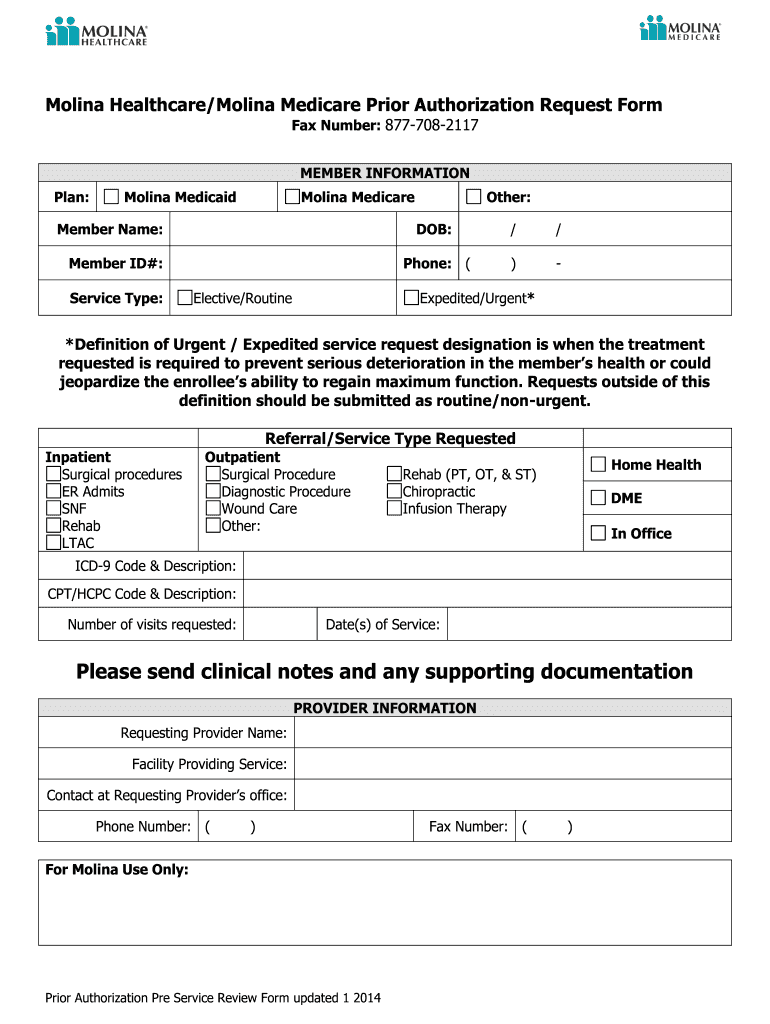
Molina Healthcare/molina Medicare Prior Authorization Request Form, Your provider must get prior. Q4 2025 prior authorization codification list.

Molina Prior Authorization 20142024 Form Fill Out and Sign Printable, Illinois marketplace pharmacy prior authorization request form. Monday through friday 8:30 a.m.
Molina Drug Prior Authorization Fill Online, Printable, Fillable, Services requiring prior authorization (revised march 2025) please note: You need a prior authorization to make sure that the care and services you receive are medically necessary.
Doing a PreCertification or Prior Authorization with Molina HealthCare, $0.00 per day for days 1 to 60 $0.00 per day for days 61 to 90 deductible $1340.00 prior authorization required for acute hospital services. Prior authorization is the process used by us to determine whether the services listed below meet evidence based criteria for medical necessity.
